How a team of unsung lab workers helped put STHS on the offensive against COVID-19
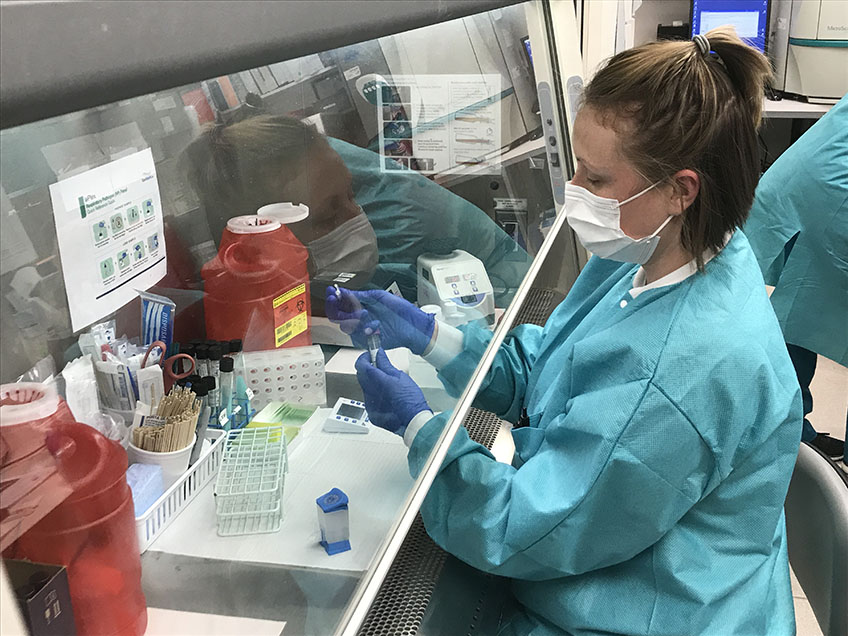
Andrea Stroo, a medical lab tech at St. Tammany Health System, processes a sample for COVID-19 testing in the laboratory at the health system’s main Covington campus. (Photo by Mike Scott / STHS)
By Mike Scott, mscott@stph.org
Numbers tell stories, and in the case of St. Tammany Health System, the daily number of COVID-19 patients listed as “patients under investigation” – that is, those suspected of having the novel coronavirus but who are awaiting test results to confirm the diagnosis – tells a doozy.
On April 2, there were 20 “PUIs,” as patients under investigation are known in medical shorthand. A day later, the number was 21. Subsequent days brought similar numbers: April 6 saw 24 PUIs. On April 7, the number was 20. There were 17 on April 8.
But then, midway through the month, something notable happened. That day – April 14, a Tuesday -- the hospital had only one PUI. Same with April 15 and 16. On April 17 and 18, there were none.
It’s not that there were fewer COVID-19 patients coming in, though. Rather, in what is being described as a watershed moment in the fight against coronavirus at St. Tammany Health System, the hospital’s lab team had fast-tracked a system to process COVID tests in-house and thus avoid the days-long logjam at already-overtaxed outside labs.
“That,” said STHS Director of Emergency Services Bradley Leonhard, “was a game-changer.”
Given how contagious the disease is, the hospital’s care teams previously had to treat all PUIs as if they were COVID-positive until tests came back. That created a drain on precious resources such as N95 masks and other personal protective equipment, to say nothing of manpower and bed space.
Thanks to in-house testing, however, that all changed literally overnight.
“In the beginning, the very first week (of the outbreak) or so, it was taking seven to 10 days to get any kind of result,” STHS Laboratory Director Judy Garic said. “It was excruciatingly painful for us, and there was nothing we could do. The labs were overwhelmed that we were sending them to -- everybody was overwhelmed. So nobody was getting results for days and days.”
Now, she said, the in-house STHS lab can provide results just 45 to 90 minutes after a test is taken.
“Knowing that has really changed the game here at St. Tammany, because there are some patients we’re testing and they’re negative and they’re not severe enough to be admitted, so they’re going home,” Garic said. “So it’s even keeping admissions from happening in St. Tammany, which is what we want to have happen: We want people to stay home and not be admitted to the hospital for this.”
Getting to that point, however, was no small feat.
According to Garic, it also speaks to the teamwork and dedication of the STHS lab team, members of which – though often overlooked as they labor away anonymously amid the centrifuges and test tubes in their laboratory at the hospital’s main Covington campus – have been working as long and as hard as anyone in the building during the COVID outbreak.
That’s evidenced by the in-house testing effort, a major win that actually required a series of smaller victories on behalf of the lab team over several very long weeks.
“It’s been extremely stressful and intense, and everybody has been doing their part,” Garic said.
Early on, a major testing hurdle was a shortage of “transport media.” That’s the technical term for the vial of fluid in which swabs are deposited to keep any virus alive for the trip to the lab after a patient is tested. Without it, there was no point in testing anybody.
But simply not testing anybody wasn’t an acceptable alternative. The doctors needed the test results in order to care properly for the patients. An anxious populace needed them, too, if for no other reason than for the assurance that something was being done to fight the virus in the community.
STHS’s solution? Its lab workers began manufacturing their own transport media to supply the Mandeville drive-through testing site the health system had established on March 16, just three days after admitting its first COVID-positive patient.
“Everybody who had any extra time, they sat there and made sample kits with the swabs and the media so that we could proceed with the drive-through testing,” Garic said. “Because it was very important to get out there into the community and let our community know we were out there, ready to test, doing what we can. So the lab has been instrumental in making those kits up that have kept the drive-through going all this time.”
Those swabs still had to be sent off to be processed, though. The real prize, Garic and her team knew, was to bring testing in-house and thus avoid the testing logjam at outside labs.
But that wasn’t as easy as it might sound, requiring a number of prerequisite steps that the lab team set about tackling.
The good news was that the lab already owned a Cepheid GeneXpert, which is the instrument – technically a “molecular assay platform” – needed to analyze specimens collected from PUIs.
Just having the machine, however, wasn’t enough to start in-house testing. So, Garic’s team set about ordering reagents, a key element in processing the collected specimens. They ordered calibration kits. They wrote up standard operating procedures and conducted the necessary training. They streamlined validation, accomplishing in five days what Garic said ordinarily takes a month or longer.
“It’s the biggest game-changer that I’ve seen in my career,” she said recently when asked to put the accomplishment into perspective. “To get this testing in our facility was an unbelievable feat that the lab achieved.”
That’s not to say there aren’t still issues. The well-publicized supply-chain problems that have affected every healthcare provider in the country have also resulted in shortages of the cartridges that, after being piped with fluid from a test, are inserted into the Cepheid GeneXpert for analysis. As a result, those cartridges on hand must be used judiciously, and efforts are constantly being made to find get new ones.
The hospital also has a handful of rapid-result testing machines that can provide results in even less time, but there’s simply no testing kits to be had for use with those. Consequently, those machines were sitting idle on a recent day.
That hasn’t stopped the lab from trying to get some, though.
“Every day, we’re fighting -- ‘Where’s our supply?’ ‘Can we get our supply?’ -- and doing everything we can to get more testing in-house so that we can better serve our patients,” Garic said.
There’s a lot of pressure involved with that. But pressure is nothing new to those in the STHS lab, who Garic said work every day on the front line of community medicine, whether in times of pandemic or times of relative normalcy.
“We’re the ones who give the diagnosis to the doctor of what’s wrong with the patient,” she said. “If the CPK is extremely high and the troponin is very high, that’s a heart attack. So, they look at the numbers we give them and that’s how they know what’s going on in your body. Without the lab, they’re just guessing.
“It’s a very big responsibility, but this is an amazing team that we have at St. Tammany. There’s techs that have been here for many, many years. They’re loyal, they’re dedicated, they will do anything for St. Tammany -- and it’s shown especially in this crisis time.”
*****
Visit STPH.org/COVID-19 for the latest information on coronavirus in St. Tammany Parish.
(Video by Tim San Fillippo / STHS)